
If you’ve lodged a workers compensation claim in NSW, you probably expect things to move quickly, especially if you’re off work and need support. But sometimes, insurers press pause. Instead of accepting or rejecting your claim right away, they may mark it as “reasonably excused.”
This doesn’t mean your claim has been denied. It simply means the insurer needs more information before they can make a decision. While this waiting period can feel frustrating, knowing why it happens and what you and your employer can do can make the process smoother.
It’s also where workplace rehabilitation providers like AusRehab step in, helping injured workers and employers keep recovery and return-to-work (RTW) planning on track, even while liability is still being worked out.
Under the NSW workers compensation law, insurers normally need to decide provisional liability within seven days of receiving a claim. If certain conditions aren’t met, the insurer may apply a reasonable excuse to delay the decision. This is a short pause to gather what is missing, not a rejection.
The pause applies to provisional weekly payments. Reasonable medical expenses will continue to be funded while the insurer collects the information it needs. For injured workers, this can be stressful, especially if you’re waiting on financial support. But knowing that this stage is part of the process can help ease concerns.
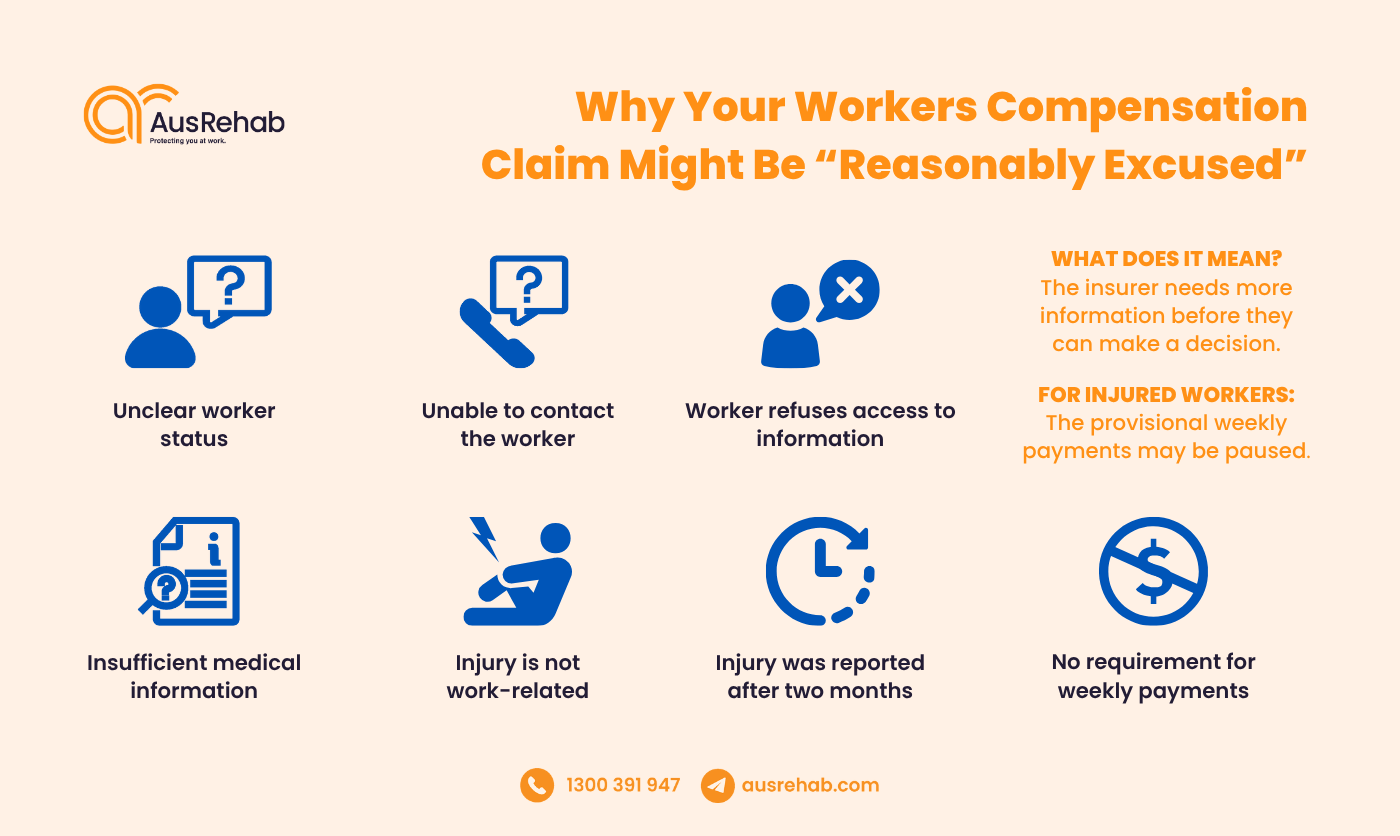
In NSW, insurers can reasonably excuse a claim if they don’t yet have enough evidence to decide on liability. This doesn’t mean the claim is rejected. It reflects the reasons for a reasonable excuse in workers compensation and allows time to gather what is missing before payments begin.
Typical reasons and what they mean:
For workers, this stage highlights the importance of clear communication and prompt paperwork. For employers, it reinforces the need to submit detailed incident reports and provide insurers with accurate information.
Here is a summary of the most common reasons and what workers and employers can do in response:
| Reason | What workers should do | What employers should do |
|
Insufficient medical information |
Ask your treating doctor to complete a clear Certificate of Capacity and send it to the insurer promptly. Keep copies of referrals and reports. | Collect and forward medical certificates quickly. Check the certificate is complete and matches roster/role details. |
| Unclear worker status | Provide payslips, contract or engagement letter, ABN status (if any), and supervisor details. | Share employment records that confirm worker status and coverage under the policy. |
| Unable to contact the worker | Confirm your phone and email with the insurer. Return calls and emails quickly. Nominate a preferred contact time if needed. | Provide up-to-date contact details (with consent). Let the worker know the insurer is trying to reach them. |
| Worker refuses access to information | Sign reasonable authorities that allow the insurer to obtain information relevant to the injury. Ask what is being requested and why. | Explain which documents are needed and how they relate to establishing liability. Limit requests to what is necessary. |
| Injury is not work-related | Give a clear description of how the injury happened and when symptoms began. Provide witness details and medical notes linking it to work. | Submit a detailed incident report and any supporting evidence (e.g., roster, location, tasks). Avoid unverified opinions; stick to facts. |
| Injury was reported after two months | Explain reasons for the delay and provide any proof of earlier notice or barriers to reporting. | Confirm when the injury was reported internally. Provide documentation that supports the timeline. |
| No requirement for weekly payments | Share evidence of incapacity or lost earnings (medical certificate restrictions, timesheets, payroll). |
Verify roster, hours, and pay records. Confirm any changes to duties or time off related to the injury. |
Notes:
Insurers may excuse a claim where there is sufficient reason to delay a decision, such as when medical evidence is missing, worker status is unclear, the worker cannot be contacted, the injury isn’t clearly work-related, or if the claim is lodged late.
If your workers compensation claim has been marked as “reasonably excused”, it can feel worrying, especially if you’re relying on payments to cover medical costs or lost wages. But remember that this is a temporary step while the insurer confirms details.
Here’s what you should expect:
3 things injured workers should do immediately:
When a claim is reasonably excused, provisional weekly payments are paused while the insurer gathers missing information. In NSW, this often means workers compensation payments may be delayed until sufficient evidence is provided.
Injured workers should provide medical and employment documents promptly and stay responsive to reduce delays, while the insurer must keep collecting evidence and decide once satisfied. Workers may also lodge a SIRA claim form, which requires a liability decision within 21 days.
When an insurer reasonably excuses a claim, employer obligations under workers compensation in NSW become critical. Fast, accurate information helps the insurer resolve uncertainty and make a decision sooner.
As an employer, your responsibilities include:
When employers are proactive, it helps the injured worker return to health and return to work more quickly. In some cases, we’ve seen a detailed incident report significantly shorten the waiting period.
Example scenario: An NSW employer lodged a detailed incident report within two days, shared CCTV clips, and sent roster and contract records that confirmed worker status. With the evidence ready, the insurer lifted the “reasonably excused” status and accepted provisional liability almost two weeks earlier than expected.
When a claim is reasonably excused, employers are still required to act responsibly. This includes submitting accurate incident reports, promptly providing relevant medical and workplace information, and cooperating fully with insurer requests. These employer obligations help minimise delays and actively support the injured worker’s recovery and return-to-work process.
Just because a claim is “reasonably excused” doesn’t mean recovery has to stall. Workplace rehabilitation providers in NSW, such as AusRehab, can offer early intervention to help both workers and employers while the insurer collects the required details.
What we do during an excused claim:
This light-touch approach ensures recovery and workplace rehab services for workers compensation are in place without waiting for a final liability decision. See more about our workplace rehabilitation services and how they support recovery at every stage of the claims process.
Workplace rehab provides early coordination and practical support. We confirm capacity with the treating doctor, outline safe duties, and prepare a simple return-to-work plan that can start when approved. This keeps everyone informed and shortens the time between decision and safe work resumption.
At AusRehab, we know that delays in workers compensation can be challenging for everyone involved. That’s why our support doesn’t stop just because a claim is reasonably excused. We continue to work with both workers and employers during this waiting period to keep recovery on track.
Early involvement centres on coordination and capacity clarification, with comprehensive assessments arranged after liability is accepted or where capacity needs further investigation.
Here’s how AusRehab workplace rehabilitation services support recovery:
AusRehab keeps recovery moving with coordinated occupational rehabilitation services in NSW. We clarify capacity with treating doctors, outline suitable or modified duties, and prepare structured return-to-work programs in NSW, so a safe plan is ready once the insurer makes a decision. Our team also guides document flow and check-ins to reduce delays.
Yes. We deliver vocational rehabilitation services in NSW, including job-seeking support, skills development, and retraining options. These services help you stay engaged and progress toward work readiness while the claim is being reviewed.
A claim being “reasonably excused” doesn’t mean recovery has to pause. Delays often stem from missing documentation, pending medical evidence, or insurer investigations. But that doesn’t stop the need for action.
During this period, both workers and employers have important responsibilities. Employers must provide accurate reports and cooperate with insurers, while workers should stay engaged in recovery planning.
This is where AusRehab support during claim liability decisions become essential. We offer early intervention, clear communication, and tailored return-to-work support while the claim is excused, ensuring recovery stays on track even during uncertainty.
✔️ Early Intervention & Injury Management
✔️ Tailored Return-to-Work Programs
✔️ Clear Communication Between All Parties
✔️ Evidence-Based Strategies for Sustainable Recovery
📞 1300 391 947
📧 office@ausrehab.com
🔗 Book a free consultation today and take the first step toward a safe, supported return to work—no matter the claim status.
An insurer may apply a reasonable excuse while it gathers missing information. They must keep documenting their efforts and make a liability decision as soon as they are satisfied. If the injured worker lodges a SIRA claim form, a decision is required within 21 days.
Provisional weekly payments are usually paused during this period, but reasonable medical expenses continue to be funded. Delays shorten when you send a complete Certificate of Capacity, accurate employment details, and respond quickly to calls or emails. Keep copies of everything you submit so follow-ups are straightforward.
Yes. Fast, accurate incident reporting and prompt delivery of rosters, position descriptions, and contact details help the insurer verify facts quickly. Employers should nominate a contact person, respond to insurer questions, and share any available evidence (for example, CCTV or witness notes). This level of cooperation often removes the reasonable excuse earlier.
You can request an internal review with the insurer, providing any new medical or factual evidence. If you still disagree, you may escalate to the Personal Injury Commission (PIC) for an independent decision. Throughout, a rehabilitation provider like AusRehab can help you plan treatment, work capacity steps, and next options.
Yes. Early workplace rehabilitation can clarify capacity with the treating doctor, recommend provisional or suitable duties, and keep communication open among all parties. This coordination means a return-to-work plan is ready to activate once a decision is made. It also reduces uncertainty and helps prevent avoidable delays.
Absolutely. AusRehab prepares graded return-to-work plans, aligns duties with current medical restrictions, and schedules check-ins to track progress. We also help gather and organise documents so the insurer has what it needs to decide sooner. This keeps recovery moving even while liability is pending.
Here at AusRehab, we streamline incident reporting, confirm role requirements and worker status, and outline safe modified duties that match medical advice. Our consultants coordinate updates with the insurer and worker, reducing rework and unanswered questions. The result is clearer documentation, fewer delays, and a smoother path to a decision.
Don’t forget to share!
Subscribe to stay updated on the latest workplace news.
Resolve your work
place injury today