When you’re involved in a workers’ compensation or personal injury claim in NSW, it’s common to come across the terms IME and IMC. Both are part of the medical assessment process, but they play very different roles in determining recovery plans, claim outcomes, and return-to-work goals.
Although they sound similar, Independent Medical Examinations (IMEs) and Injury Management Consultations (IMCs) serve different purposes. Understanding the difference between IME and IMC can help you stay informed, reduce confusion during your claim, and optimise the rehabilitation process.
At AusRehab, our workplace rehabilitation consultants regularly support both IMC and IME processes for injured workers to receive fair, coordinated, and sustainable return-to-work outcomes.
In the NSW workers’ compensation system, both IME (Independent Medical Examination) and IMC (Injury Management Consultation) play important roles in guiding recovery, assessing capacity, and supporting claim decisions. While they’re often mentioned together, the difference between IME and IMC in NSW lies in their purpose and timing.
An IMC focuses on collaboration, where the treating doctor, employer, and insurer come together (with help from a SIRA-approved Injury Management Consultant) to clarify work capacity, resolve certification issues, and address barriers to return-to-work (RTW).
An IME, on the other hand, provides an independent medical opinion when there’s uncertainty about diagnosis, treatment, or entitlements. It’s carried out by a specialist who isn’t involved in the worker’s treatment and is used when more evidence is needed to make a fair decision.
Sometimes, the case manager may find that the available medical evidence is unclear. Following SIRA Guidelines, they first work with the treating parties to gather the right information. If questions remain, they may request an independent opinion to help confirm whether treatment or liability is reasonably necessary. This ensures every decision is based on objective and reliable evidence.
An IMC is a collaborative meeting that helps resolve return-to-work issues through discussion and alignment between the treating doctor, employer, and insurer. An IME is an independent assessment by a specialist who provides an impartial medical opinion to support claim decisions.
In short:
An Injury Management Consultation (IMC) is a collaborative medical consultation used in NSW workers’ compensation to support a worker’s recovery and return-to-work goals. It involves the Injury Management Consultant (IMC doctor), the Nominated Treating Doctor (NTD), the employer, and the insurer working together to clarify capacity, certification, and any barriers that may delay progress.
Unlike an independent medical assessment, an IMC complements the treating doctor’s ongoing care. It focuses on aligning all parties on the worker’s current capacity for work and identifying suitable duties that support a safe and sustainable return to work.
A case manager may arrange an IMC when there are ongoing differences between the treating doctor, employer, and worker about medical certification or recovery expectations. During the session, the IMC may review medical information, discuss concerns with the treating team, and provide written recommendations to guide recovery planning.
If agreement is reached, a revised Return-to-Work Plan is developed and implemented. When issues remain unresolved, such as conflicting opinions or workplace barriers, the case manager may then consider an Independent Medical Examination (IME) or, in more complex cases, referral to the Personal Injury Commission (PIC) for formal review.
An IMC is often organised when a workers’ compensation claim faces delays caused by unclear medical advice, inconsistent certificates, or poor communication between stakeholders. The IMC referral process in NSW helps clarify these issues early, reducing disputes and keeping recovery plans on track.
An IMC for return-to-work is particularly helpful when:
Example: If two medical certificates conflict, an IMC ensures all parties align before an IME is even considered.
An IMC report on workers’ compensation provides clear recommendations on recovery and capacity, ensuring that decisions are collaborative, timely, and in the best interest of both the worker and employer.
An Independent Medical Examination (IME) is an objective medical assessment carried out by a specialist who is not involved in the worker’s treatment. In NSW workers’ compensation, an IME provides an independent opinion on the worker’s diagnosis, capacity for work, treatment needs, or level of permanent impairment. It helps insurers make fair and evidence-based decisions about recovery, entitlements, and next steps.
A case manager arranges the assessment in line with the SIRA Guidelines on Independent Medical Examinations and Reports. The reason for referral must be clearly defined, and the worker, nominated treating doctor, and employer are notified in writing at least 10 working days before the appointment. The IME specialist is chosen based on their qualifications and relevant clinical expertise.
After the assessment, the findings are detailed in an IME report (NSW), which guides treatment approvals, compensation decisions, and recovery planning. If the report supports that treatment or surgery is reasonably necessary, it is approved and communicated to all parties. If not, the case manager provides a written explanation and outlines available review or appeal options.
According to SIRA Independent Medical Examinations Fact Sheet, IMEs must be performed impartially, ensuring workers are treated respectfully and reports are delivered within set timeframes to keep claims moving smoothly.
An IME is used when additional, objective medical evidence is needed to support a workers’ compensation or personal injury claim. Unlike an IMC, which focuses on collaboration, an IME provides an independent specialist opinion to help insurers make fair, evidence-based decisions about treatment, liability, or entitlements.
The IME referral process in NSW is typically initiated when the treating doctor’s reports are unclear, inconsistent, or unavailable. It ensures that every claim decision is backed by accurate, specialist medical advice and complies with SIRA’s guidelines.
An IME medical assessment in NSW is usually requested when:
The findings are documented in a formal IME report (NSW), which helps guide decisions about treatment, work capacity, and compensation.
In some cases, the case manager may also engage SIRA-approved Independent Consultants such as physiotherapists, chiropractors, osteopaths, or psychologists. Their input helps verify the reasonable necessity of ongoing allied-health treatment, supporting consistent, evidence-based care for injured workers.
While both IMC and IME play vital roles in NSW workers’ compensation, they serve very different purposes in managing recovery and claim decisions. The main difference lies in their timing, purpose, and approach.
Below is a table of comparison showing the difference between IME and IMC in NSW:
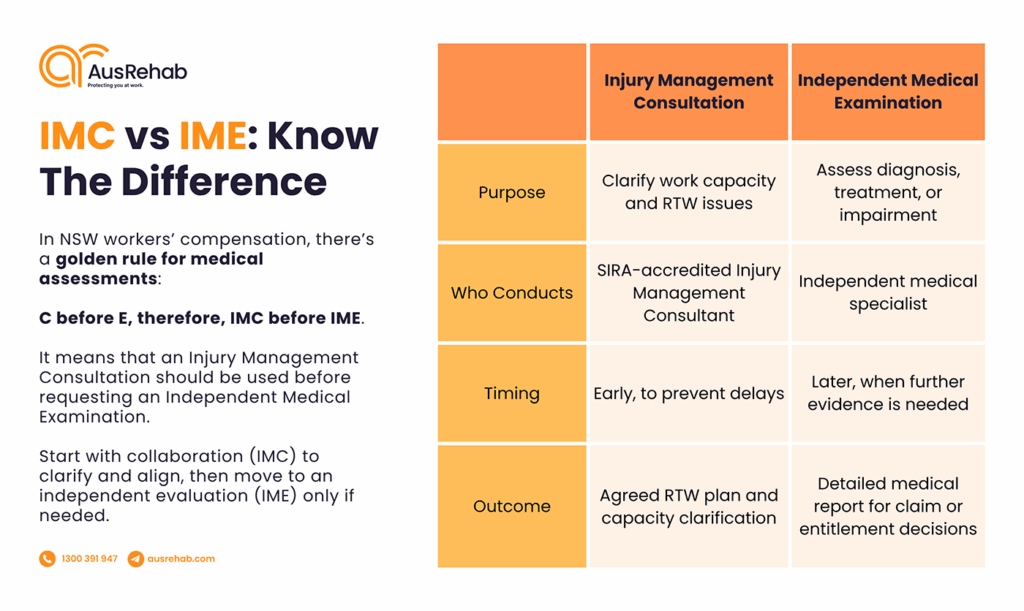
To put it simply, the rule of thumb is “C before E” — IMC before IME.
Insurers are encouraged to use collaborative solutions first before seeking independent medical opinions, ensuring decisions are fair, transparent, and efficient.
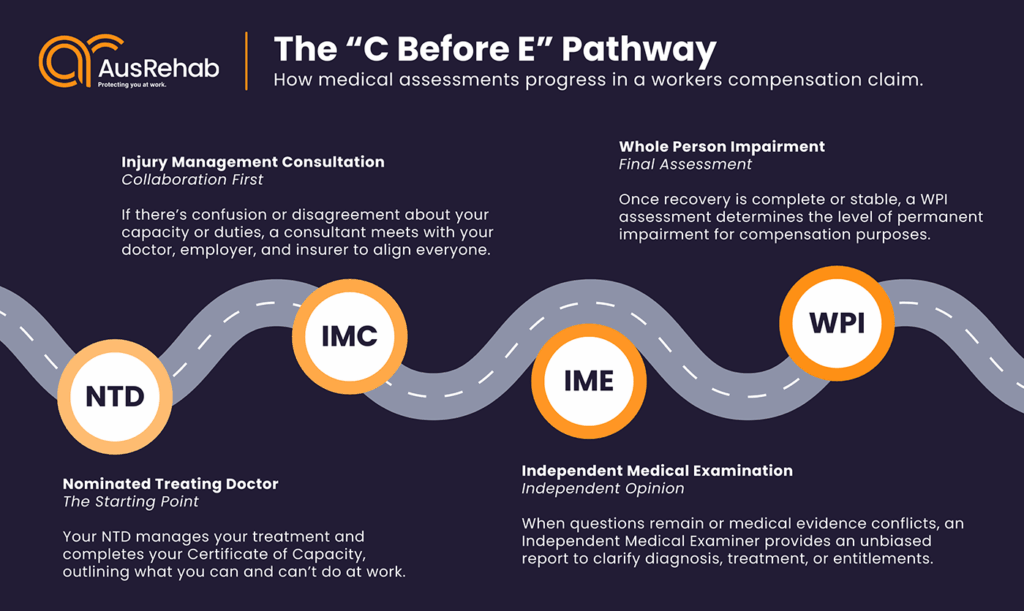
If an IMC doesn’t resolve the concern, the case may progress to an IME for further review. When disputes still remain, the matter can be referred to the Personal Injury Commission (PIC) for mediation or formal medical assessment.
This structured pathway — IMC first, IME second, PIC if needed — ensures every chance for early resolution while still providing access to impartial review if required.
An IMC is completed before an IME because it aims to fix issues through communication and cooperation first. If the IMC successfully clarifies capacity, certification, or workplace duties, an IME may no longer be necessary. This C before E approach saves time, reduces costs, and helps everyone stay focused on safe and sustainable recovery.
IMEs and IMCs have distinct roles in the workers’ compensation system. While an IMC focuses on early collaboration between the worker, employer, and treating doctor to resolve medical or return-to-work barriers, an IME provides an independent medical opinion when disputes or complex issues arise.
When used appropriately, both processes contribute to better recovery and claim outcomes:
Both IMC and IME processes aim to support recovery, but in different ways.
At AusRehab, we make every medical and workplace assessment part of a worker’s recovery journey, not an obstacle to it. As a leading workplace rehabilitation provider in NSW, we ensure that both IMC and IME processes are managed efficiently, resulting in fair, timely, and safe outcomes.
Here’s how we support both processes:
Through this collaborative model, AusRehab ensures that IMC and IME processes are not just procedural steps but meaningful interventions that guide effective decisions.
AusRehab ensures both IMC and IME processes are handled smoothly and effectively. For IMCs, we coordinate the referral, facilitate communication between parties, and make sure all documentation supports early resolution. For IMEs, we help prepare evidence, clarify medical history, and ensure recommendations are integrated into a recovery plan that benefits all stakeholders.
Understanding the IME vs IMC difference is essential for achieving fair, evidence-based outcomes in workers’ compensation. Both processes serve unique but complementary roles in managing recovery and claim progress.
An IMC focuses on early collaboration, helping resolve barriers to return-to-work, clarify medical advice, and keep all parties aligned. An IME, meanwhile, offers independent validation to confirm that treatment, capacity, or entitlement decisions are supported by objective medical evidence.
Together, they ensure every claim is managed with clarity, fairness, and accountability:
IMC = early collaboration and faster recovery
IME = independent evidence and fair outcomes
At AusRehab, we support both processes by fostering communication between treating teams, insurers, and employers that every assessment contributes to better recovery outcomes and fair claim resolutions.
Contact AusRehab’s workplace rehabilitation team to ensure your next assessment supports faster recovery and fair claim outcomes.
📞 1800 991 614
📧 office@ausrehab.com
🔗 Book a consultation to discuss your IMC or IME coordination needs, and let AusRehab guide your next step toward a safe and successful recovery.
An Injury Management Consultation (IMC) is a collaborative medical consultation under the NSW workers’ compensation system. It involves the Injury Management Consultant (IMC doctor), the Nominated Treating Doctor (NTD), the employer, and the insurer working together to clarify work capacity, address recovery barriers, and plan a safe return to work.
An IMC is used when there’s uncertainty or inconsistency in medical certificates, workplace adjustments, or a worker’s capacity for duties. It helps align all stakeholders early in the claim, preventing delays and supporting faster recovery. For example, if two certificates conflict, an IMC helps resolve the issue before an Independent Medical Examination (IME) is needed.
An Independent Medical Examination (IME) is an objective medical assessment conducted by a specialist who isn’t involved in the worker’s treatment. It provides an independent medical opinion on diagnosis, treatment, or work capacity to help insurers make fair and evidence-based decisions about workers’ compensation claims in NSW.
An IME is required when medical evidence from the treating parties is unclear, inconsistent, or unavailable. It’s often used to confirm liability, surgical recommendations, or impairment ratings, such as during a Whole Person Impairment (WPI) assessment. The IME referral process in NSW follows SIRA Guidelines to ensure fairness and transparency.
After the IME report is received, the case manager reviews the findings to guide claim decisions. If the IME supports the proposed treatment or procedure as reasonably necessary, it’s approved and communicated to all parties. If not, the case manager explains the rationale in writing and outlines available review or appeal options for the worker.
In NSW, an IMC is usually arranged by the insurer or employer in collaboration with the Nominated Treating Doctor (NTD). An IME, however, is requested by the insurer when independent medical evidence is needed to clarify diagnosis, treatment, or entitlement decisions under the workers’ compensation system.
Yes. An IMC aims to resolve issues early through open communication between the treating doctor, employer, and insurer. When successful, this collaboration often eliminates the need for an IME, saving time, reducing stress, and keeping recovery plans on track. This is why SIRA encourages the “C before E” approach, IMC before IME.
Not necessarily. An IME may take additional time to schedule and report, but it ensures that complex or disputed claims are resolved fairly and based on independent medical evidence. By using an IMC first to clarify simple issues, insurers often reduce the need for lengthy IME referrals and keep claims progressing smoothly.
Don’t forget to share!
Subscribe to stay updated on the latest workplace news.
Resolve your work
place injury today