Prefer to Listen? Play this quick summary instead!
Car accidents not only affect the body, but they can also affect how a person feels, thinks, and responds to everyday situations. The mental impact of a car accident often shows up quietly, sometimes days or weeks after the crash. Many people feel unsettled, tense, or unsure about driving again, even when physical injuries are mild or have healed.
These reactions are common and human. The brain reacts to sudden danger by trying to protect you. That response can linger and shape mood, sleep, focus, and confidence. This does not mean something is wrong with you. It means your nervous system is adjusting after a shock.
Understanding mental health after a car accident helps people make calmer and safer decisions. It also answers a question many people hesitate to ask: “Am I safe to drive again?” With the right information and support, recovery can move forward with clarity, confidence, and care.
Can a Car Accident Affect Your Mental Health?
Yes. A car accident can affect mental well-being even when physical injuries are minor or not present. The psychological impact of a car accident often comes from the sudden shock and loss of control during the event. The brain reacts to danger quickly, and that response does not always switch off once the crash is over.
These reactions are common and expected. They are not a sign of weakness. Many people experience emotional or cognitive changes without realising they are linked to the accident. The effects may appear straight away or develop gradually over the following weeks. This delayed response can feel confusing, especially when the body seems fine.
Psychological Injuries Can Occur Without Physical Harm
A collision does not need to be severe to cause distress. Even low-speed crashes can trigger mental trauma from a car crash. The mind remembers the threat, not the damage. People may feel unsettled, alert, or uneasy without understanding why. These reactions often settle with time and support.
Common Areas Affected
After an accident, changes may appear in everyday functioning. Mood can shift. Sleep may become lighter or disrupted. Concentration can drop during routine tasks. Stress tolerance may feel lower than usual. Confidence in driving or travelling in vehicles often reduces.
What is psychological trauma after a car accident?
Psychological trauma after a car accident refers to the emotional and mental responses that follow a sudden, threatening event. It reflects how the brain processes danger and adapts afterwards, not a diagnosis or label.
Common Mental Health Symptoms After a Car Accident
Emotional and cognitive reactions often appear soon after a crash. These responses are the body’s normal reaction to stress and threat. They can happen even when injuries are minor. People often experience emotional or mental changes without immediately realising those changes are caused by the accident. Recognising early signs helps people respond calmly and seek support if needed.
Early and Common Reactions
- Feeling on edge or jumpy, especially near traffic
- Trouble sleeping after a car accident, including light or broken sleep
- Intrusive thoughts after a crash, such as sudden memories or mental images
- Fear of driving after an accident, or avoiding being a passenger
- Irritability, tearfulness, or sudden mood changes
These symptoms often settle over time. For some people, they linger or interfere with daily activities. That does not mean something is wrong. It means the nervous system is still adjusting.
When Mental Health Symptoms May Need Extra Support
Most emotional responses after a car accident ease with time. Some signs suggest extra support may help recovery move forward. These signs do not mean something is wrong. They show the nervous system is still under strain and needs guidance. Early support can protect safety, confidence, and daily functioning.
People often hesitate because they worry about labels like Post-traumatic Stress Disorder (PTSD) after a car accident. Diagnosis is not the starting point. The focus is on how symptoms affect everyday life, especially driving, work, and concentration. Changes such as panic symptoms when driving or repeated nightmares after a car accident can signal that stress responses are not settling on their own.
Signs It May Be Time to Seek Support
Signs That Psychological Support May Be Required
| Sign | Why It Matters |
|---|---|
| Nightmares or flashbacks | Trauma responses are not settling |
| Panic near traffic | Safety and driving confidence are affected |
| Strong avoidance | Work, travel, or routines are disrupted |
| Ongoing low mood | Emotional well-being is impacted |
| Concentration issues | Driving awareness and decision-making are reduced |
Support at this stage is about stability and confidence. It helps people understand what they are experiencing and decide on safe next steps. Remember, only a qualified health professional can diagnose conditions such as PTSD, anxiety, or depression. Seeking support is about understanding symptoms and protecting recovery, not applying a diagnosis.
Why Car Accidents Can Affect Mental Health
Car accidents trigger a powerful stress response after an accident. The body reacts first to protect safety. This response is fast and automatic. It does not depend on injury severity. Even low-speed crashes can activate the same system.
The Brain’s Stress Response
A collision signals a sudden threat. The brain activates fight-or-flight. Heart rate rises. Muscles tense. Attention narrows. These reactions help people respond in danger. They are normal and protective at the time.
Why the Nervous System May Stay in “Alert Mode”
After the crash, the trauma response nervous system can remain on high alert. The brain learns that driving or traffic equals risk. This learned response can trigger anxiety in similar situations later. Busy roads, loud noises, or near-misses can reactivate the stress response. The body responds as if danger is present again.
This pattern explains why anxiety can appear days or weeks later. It also explains why people feel jumpy, tense, or unsure behind the wheel. These reactions reflect the nervous system trying to prevent harm. They are common and understandable after a crash.
Why do car accidents cause anxiety or trauma?
Because the brain links the accident with danger and keeps the body alert to protect safety. With time and support, this response can settle and confidence can return.
How Mental Trauma Can Affect Driving Ability
Mental trauma can change how the brain processes information on the road. Trauma affecting driving often shows up as changes in attention, confidence, and reaction speed. These changes can affect safety, even when physical injuries have healed. The brain stays alert to perceived risk, which can make driving feel harder than before.
Common Driving Impacts
- Reduced attention and scanning during complex traffic situations
- Slower reaction time at intersections or sudden stops
- Feeling overwhelmed in traffic, especially in busy or unfamiliar areas
- Hypervigilance driving, where constant alertness leads to fatigue
- Loss of driving confidence, including hesitation or avoidance
These reflect a protective stress response. The mind focuses on threat detection. This can narrow attention and drain energy over time. Fatigue and reduced focus can follow, especially on longer drives.
💡 These are normal trauma responses, not a personal weakness. Many people experience them after a crash. With support and gradual exposure, driving confidence and safety can improve.
PTSD, Anxiety, and Depression After Car Accidents
Emotional responses after a crash exist on a wide spectrum. PTSD after a car accident, anxiety after a crash, and depression after a car accident can affect people differently. These experiences are not limited to major collisions. They can follow minor or moderate incidents as well.
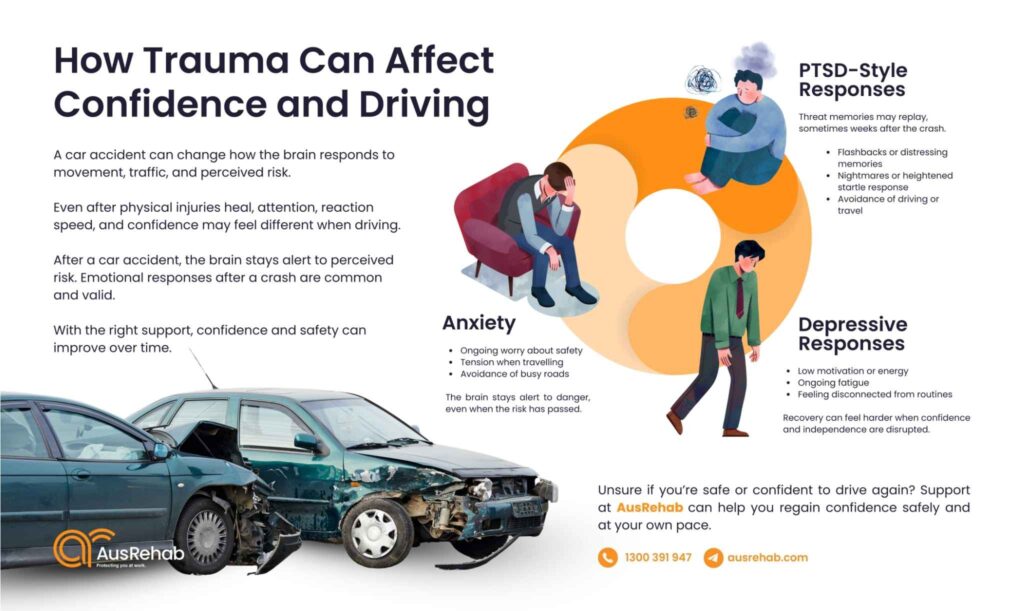
Anxiety After a Crash
- Constant worry about safety or future accidents
- Physical tension in the body, especially when travelling
- Fear of traffic, intersections, or busy roads
Anxiety often reflects the brain staying alert to perceived danger. This response can persist even when the risk has passed.
PTSD-Style Symptoms
- Constant worry about safety or future accidents
- Physical tension in the body, especially when travelling
- Fear of traffic, intersections, or busy roads
These symptoms relate to how the brain stores and replays memories of danger. They can appear days or weeks after the event.
Depression After a Car Accident
- Constant worry about safety or future accidents
- Physical tension in the body, especially when travelling
- Fear of traffic, intersections, or busy roads
Depression can develop when recovery feels slow or when confidence and independence are affected.
Myth-Busting Points:
- PTSD is not limited to severe crashes
- Symptoms may develop weeks later
- Emotional injury is valid even if the body heals
Emotional recovery deserves the same care and attention as physical healing.
When to Get Help After a Car Accident
Knowing when to get help after a car accident can feel unclear, especially when physical injuries seem minor or have healed. Mental and emotional recovery often follows a different timeline. Paying attention to how symptoms affect daily life helps guide the next step.
Consider Support If Symptoms Are:
- Persistent, lasting longer than expected
- Interfering with daily activities, work, or relationships
- Affecting driving confidence or safety, even on short or familiar trips
These signs suggest the nervous system has not fully settled. Support at this stage focuses on safety, confidence, and gradual recovery.
Why Early Support Matters
Early mental health support after a crash helps the brain and body reset. It improves recovery by addressing symptoms before they become entrenched. It supports independence by rebuilding confidence in daily activities. It also helps people make informed decisions about driving, work, and routine tasks.
How AusRehab Supports CTP Clients After Car Accidents
Recovering after a car accident often involves more than physical healing. CTP rehabilitation support focuses on helping people regain safety, confidence, and independence in everyday life, including driving. AusRehab provides practical, OT-led support that aligns recovery with real-world demands.
Occupational Therapy Driving Assessments
An OT driving assessment after an accident looks at readiness, attention, and safety. The focus stays on how mental and physical symptoms affect driving tasks. Barriers such as anxiety, reduced concentration, or slower responses are identified early so risks can be managed.
Driving Rehabilitation Programs
A driving rehabilitation program supports gradual confidence rebuilding. Exposure is paced and safety-focused. Skills are strengthened step by step, with strategies that help people return to driving without feeling overwhelmed.
Vehicle Driving Ergonomics and Modifications
Poor setup can increase fatigue and discomfort. Vehicle driving ergonomics address seating position, controls, and posture. Small adjustments often improve comfort, alertness, and safety behind the wheel.
Activities of Daily Living (ADL) Support
Recovery extends beyond driving. ADL assessment supports daily tasks such as shopping, household activities, and community access. The goal is to restore independence while respecting current limits.
Coordinated Care
Support is coordinated with GPs, insurers, and treating providers. Clear communication keeps recovery aligned and reduces uncertainty during the CTP process.
Driving Impact vs OT Support
Driving Challenges and How Occupational Therapy Support Helps
| Driving Challenge | How OT Support Helps |
|---|---|
| Reduced attention | Structured driving assessment |
| Panic in traffic | Gradual exposure strategies |
| Fatigue | Ergonomic adjustments |
| Loss of confidence | Rehabilitation planning |
Support That Helps You Regain Confidence Safely
Car accidents can have lasting mental and emotional effects, even when physical injuries are minor or have healed. Anxiety, reduced confidence, and uncertainty around driving are common responses after a crash. These reactions are normal and understandable.
Recovery works best with clear guidance and practical support. Early help supports informed decisions about driving, daily activities, and safety. It also protects independence and long-term well-being during recovery.
AusRehab supports people recovering after motor vehicle accidents through practical, OT-led assessments and rehabilitation. Care stays focused on safety, confidence, and clear communication with GPs, insurers, and treating providers.
If you feel unsure about driving or daily activities after a car accident, support is available. Early guidance leads to safer outcomes and stronger recovery.
Frequently Asked Questions (FAQs)
Can a car accident affect your mental health even if injuries are minor?
Yes. Emotional and psychological responses can occur after any car accident, including minor collisions. The nervous system responds to perceived threat, not injury severity. Symptoms may appear immediately or develop weeks later.
What mental health symptoms are common after a car accident?
Common mental health symptoms after a car accident include anxiety, sleep disturbance, intrusive thoughts, avoidance of driving, and mood changes. These reactions reflect stress recovery, not personal weakness, and are a common part of adjustment after a crash.
Can mental trauma affect your ability to drive safely?
Yes. Trauma can affect attention, reaction time, and confidence. These effects are common and treatable with the right guidance and support.
How can mental trauma affect driving ability?
Mental trauma can reduce attention, slow reaction time, and increase fatigue or overwhelm in traffic. Some people also experience avoidance or loss of confidence. These are normal trauma responses that can improve with support.
Can PTSD develop after a minor car accident?
Yes. PTSD-style symptoms can develop after minor or moderate accidents. Trauma is related to how the event is experienced, not how severe the crash appears. Only a qualified health professional can diagnose PTSD.
How do I know if I’m safe to drive again after a crash?
You may be ready to drive again when you can focus, react calmly, and manage traffic without fear or overwhelm. If anxiety, reduced attention, or hesitation affects your safety, a professional assessment can help. An occupational therapist can assess readiness and guide safe next steps.
Is it normal to feel scared to drive after a car accident?
Yes. Fear or hesitation when driving is a common response after a crash. The brain may stay alert to danger as a protective response. This does not mean you are unsafe or incapable of driving.
When should I seek help after a car accident?
Consider support if emotional symptoms persist, interfere with daily activities, or affect your confidence or safety when driving. Early guidance can support recovery and help you make informed decisions.
What is an OT driving assessment after a car accident?
An OT driving assessment reviews physical ability, attention, confidence, and reaction skills related to driving. It identifies barriers that may affect safety and recommends strategies, supports, or rehabilitation where needed. The goal is informed and safe decision-making, not judgment.
How does AusRehab support CTP clients after car accidents?
AusRehab supports CTP clients with OT-led driving assessments, rehabilitation programs, and domestic assistance. Care focuses on safety, confidence, and gradual return to independence. Support is coordinated with GPs, insurers, and treating providers to keep recovery clear and structured.