Referral and Onboarding Process for Insurers
Referring is simple. We acknowledge all insurer workplace rehab referral form submissions within 1 business day.
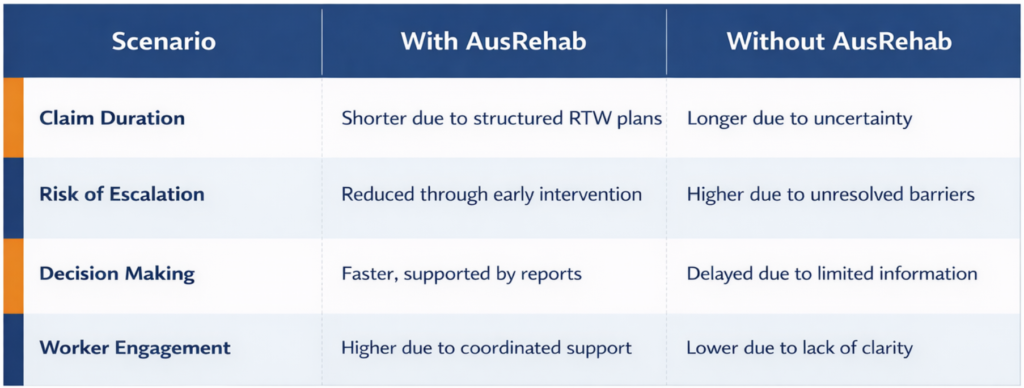
AusRehab delivers outcomes-focused workplace rehabilitation for insurers and case managers under the NSW Workers’ Compensation and CTP schemes. We help reduce claim duration, clarify work capacity, and support timely, safe return-to-work outcomes with assessments and plans that are practical, evidence-based, and insurer-ready.

We provide independent functional assessments, clear reporting, and intervention strategies that improve decision-making and resolve claims faster. Our approach identifies risks early, supports collaboration, and removes barriers that prevent progress.

As a SIRA-approved workplace rehabilitation provider, we understand the pressure on insurers to manage claims fairly, efficiently, and within scheme expectations.
Our team helps clarify capacity, reduce barriers, and support safe RTW outcomes with minimal delays.

✅ Work capacity clarity: Clear understanding of worker abilities and restrictions.
✅ Early risk detection: Identification of psychosocial and workplace barriers.
✅ Faster decisions: Timely, structured reports aligned with insurer communication requirements.
✅ Reduced claim duration: Strategic RTW planning and measurable goals.
✅ Better worker engagement: Improved cooperation and clarity for injured workers.
✅ Scheme compliance: Assessments and reports aligned with SIRA, Workers Comp, and CTP standards.
AusRehab delivers end-to-end services that support liability decisions, clarify work capacity, and create evidence-based plans for return-to-work and long-term employment success.
The Initial Needs Assessment is your first step toward clarity. We look at injury details, worker capacity, and recovery barriers to give you a clear snapshot of what’s possible and what’s next.
This work capacity assessment for insurers identifies:
🔎 What Insurers Gain from the INA:
Case management for workers returning to their original employer provides structured, early intervention support that aligns capacity with workplace demands.
AusRehab’s same-employer case management includes:
These services reduce uncertainty, help keep workers engaged with meaningful activity, and support efficient claim management under workers’ compensation NSW standards.
For injured workers who are unable to return to pre‑injury roles with their original employer, AusRehab provides vocational pathways for workers’ compensation claims that support transition into new employment.
This includes:
This service is ideal for cases where long‑term injury effects require a fresh work environment or new career direction.
Our Workplace Assessment service analyses job tasks, environments, risks, and supports. We identify workplace barriers that affect return-to-work and suggest reasonable adjustments to enable employees to perform their duties.
This helps prevent escalation and promotes a sustainable RTW plan.
A detailed Functional Capacity Evaluation provides objective measures of a worker’s physical and functional abilities. These evaluations:
Use FCEs to understand how it guides insurers in decision-making and provide clarity on next steps.
We create a plan that aligns with medical advice and the demands of the workplace. Every return-to-work plan includes duties, upgrade paths, timelines, and check-ins. These are easy to understand and align with insurer and scheme requirements.
This service helps reduce claim duration and supports safe and sustainable return-to-work outcomes.
Our Activities of Daily Living (ADL) assessment service evaluates how an injury impacts daily living functional capacity. This informs:
This is especially important for long-term or high-risk cases.
We conduct Vocational Assessment that produces:
We complement this with Labour Market Analysis to ensure vocational outcomes are realistic, sustainable, and well-supported.
Referring is simple. We acknowledge all insurer workplace rehab referral form submissions within 1 business day.
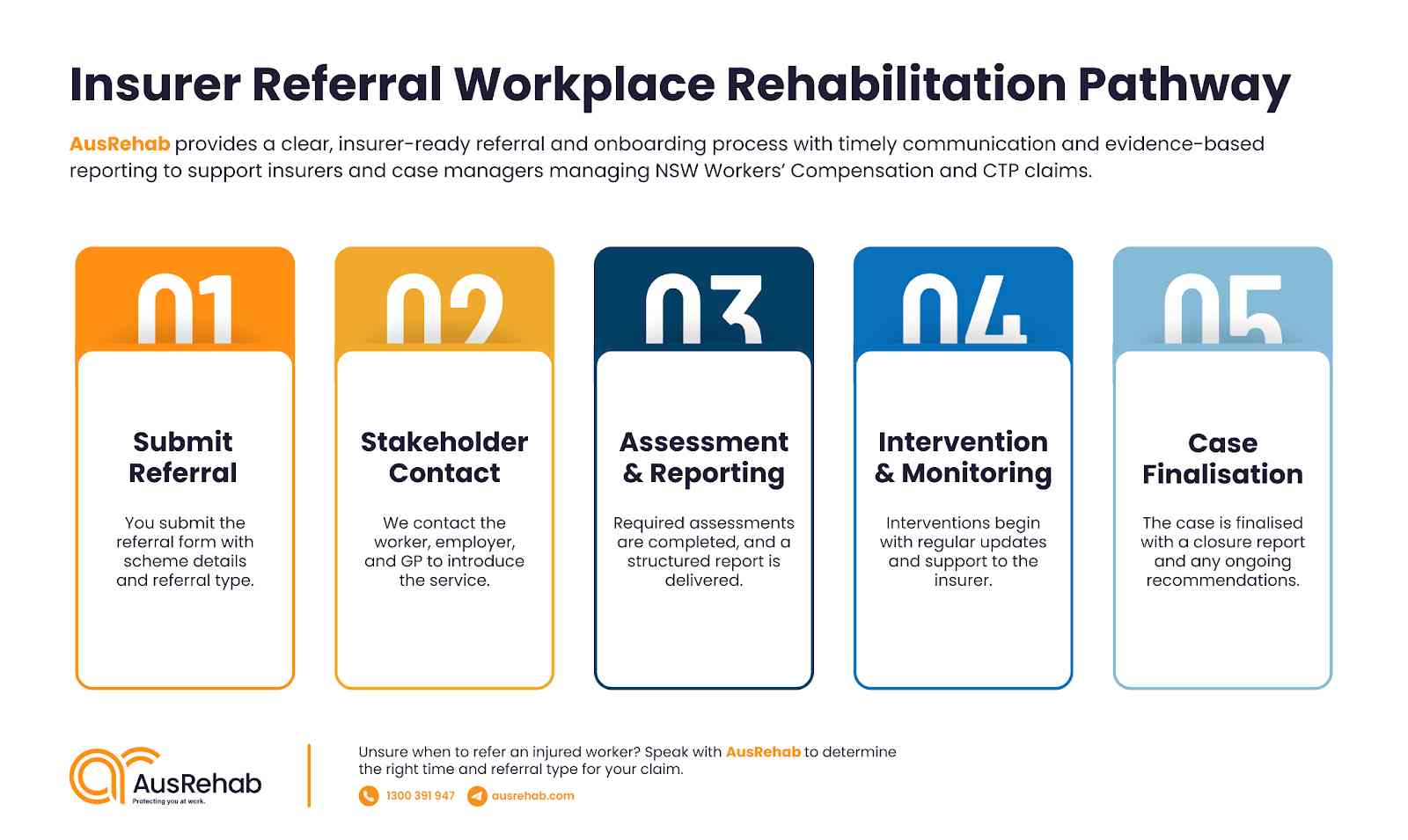
To refer, complete our insurer workplace rehab referral form below. All referrals are acknowledged within one business day.
You can download our AusRehab Referral Form (PDF) and email the completed form with supporting documents to office@ausrehab.com

🔒 All information is handled confidentially and in line with privacy legislation.
AusRehab is a proven, SIRA-approved workplace rehabilitation provider with deep experience in both Workers’ Compensation and CTP schemes across NSW.
✅ Strong track record in early intervention workplace rehabilitation
✅ Success in managing complex claims in workplace rehabilitation
✅ Timely, transparent communication with stakeholders
✅ Evidence-based, scheme-compliant reporting
✅ Collaborative approach with treating teams and employers
✅ NSW-wide service capability and flexibility
Contact us directly on 1300 391 947
A workplace rehabilitation provider supports insurers and case managers by assessing work capacity, identifying barriers to recovery, and developing structured return‑to‑work plans.
AusRehab delivers independent, evidence‑based assessments and clear reports that help insurers make informed decisions around liability, treatment direction, and suitable duties. The focus is on reducing uncertainty, improving communication, and supporting timely claim progression.
Workplace rehab reduces claim duration and costs through early intervention, clear capacity clarification, and structured planning. By identifying functional limits and psychosocial or workplace barriers early, insurers can avoid delays, unnecessary treatment extensions, and claim escalation. Clear RTW goals, timeframes, and monitoring help keep claims on track and reduce long‑term exposure.
An insurer should refer a claim as early as possible when there is uncertainty around capacity, delayed recovery, workplace barriers, or risk of escalation. Early referral is also appropriate when a worker has reduced duties, extended time off work, psychosocial risk factors, or difficulty engaging with the employer or treating team. Early workplace rehabilitation often leads to better outcomes and faster resolution.
A workplace rehabilitation report typically includes:
Reports are structured to support insurer decision‑making and align with scheme requirements.
Functional Capacity Evaluations provide objective data on a worker’s physical and functional abilities. For insurers, FCEs help clarify what tasks a worker can safely perform, support liability and work capacity decisions, and guide RTW or vocational planning. They are particularly valuable in complex or disputed claims where objective evidence is required.
Workplace rehabilitation identifies psychosocial and workplace barriers through structured assessment, worker engagement, and employer consultation. Barriers such as fear of re‑injury, low confidence, poor communication, or unsuitable duties are addressed early through education, graded duties, and coordinated planning. Early identification reduces the risk of prolonged claims and disengagement.
Yes. Workplace rehabilitation is highly effective for complex or high‑risk claims. AusRehab regularly supports claims involving prolonged time off work, psychological factors, multiple injuries, or failed RTW attempts. Through structured assessment, clear planning, and consistent communication, complex claims are stabilised and guided toward realistic, sustainable outcomes.
Workplace rehab improves RTW outcomes by aligning capacity, duties, and medical advice. Clear plans, regular monitoring, and collaboration with employers and treating practitioners help workers return safely and with confidence. This coordinated approach improves engagement, reduces setbacks, and supports sustainable work participation.
When submitting a referral, insurers are typically asked to provide:
All referrals are acknowledged within one business day.
Yes. AusRehab supports claims under both the NSW Workers Compensation Scheme and the NSW CTP Scheme. Our services are delivered in line with scheme expectations and reporting requirements, ensuring compliance and consistency for insurers and case managers.

Start improving claim outcomes with AusRehab today. Use the insurer workplace rehab referral form and email it to office@ausrehab.com.
For urgent or complex cases, contact us directly on 1300 391 947.